
Blog: The Role of Genomics in Alzheimer’s Disease
Alzheimer’s disease is a debilitating neurodegenerative disorder that affects millions of people across the globe. While the cause of Alzheimer’s is still unknown, recent advances in genomics and whole exome sequencing are helping to shed light on the underlying biology of the disease. In particular, large-scale genome sequencing efforts have identified some genes that are associated with an increased risk of developing Alzheimer’s. By understanding the role these genes play in the disease, researchers hope to develop better treatments and eventually a cure for Alzheimer’s.
What is Alzheimer’s Disease?
Alzheimer’s is classified as a progressive neurodegenerative disorder and is characterized by severe memory loss, cognitive decline, and changes in mood and behavior. Further along in its progression, it may lead to problems with movement and bodily function as well. Alzheimer’s is the leading cause of 60-80% of all dementia cases and can be distinguished by mild cognitive impairment that occurs as an early symptom. Alzheimer’s not only impairs memory, thinking, and decision-making but also ranks as the sixth leading cause of death in the US
Brief History of Alzheimer’s
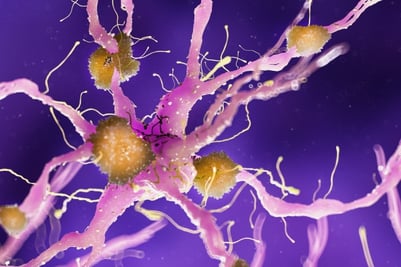
In 1906, German physician Alois Alzheimer described the peculiar case of a patient who displayed extensive memory loss, irrational suspicions about her family, and other rapidly deteriorating psychological changes. Even more strange, however, was the dramatic shrinkage in nerve cells and abnormal deposits (later identified as amyloid beta proteins) around nerve cells that Dr. Alzheimer saw in the patient’s autopsy. In 1910, a colleague named Emil Kraepelin officially coined the affliction as “Alzheimer’s Disease” in the eighth edition of his book Psychiatrie.
Awareness and understanding of the disease advanced greatly in the century after Dr. Alzheimer’s passing in 1915. Rapidly advancing imaging technology and reliable behavioral measures have clarified both the biological and psychological symptoms of Alzheimer’s. This led families and loved ones of those affected to form awareness associations such as the Alzheimer’s Association and ISTAART.
The Role of Genomics
Genomic information may help with early detection, prevention, and the creation of powerful pharmaceutical remedies for Alzheimer’s. From a genomics standpoint, the most promising area of research involves pinpointing genes that may influence an individual’s risk for developing the disorder—whole exome sequencing.
In recent years, genome-wide association studies (GWAS) have identified some potential risk genes—many of which encode proteins involved in neuron communication and synaptic plasticity. By better understanding how these genes interact with each other and the environment, researchers hope to develop more targeted treatments that could delay or even prevent Alzheimer’s from developing.
Alongside GWAS, bioinformatics is playing an increasingly important role in advancing the understanding of Alzheimer’s. New multi-omics approaches, such as transcriptomics, proteomics, and epigenomics, have identified novel signatures that may be linked to an increased risk of Alzheimer’s [1]. This data, in turn, is helping researchers shed light on the underlying biological mechanisms of the disorder and creating greater opportunities for developing treatments and a cure.
Detection and Prevention
Early onset Alzheimer’s disease, which has a Mendelian inheritance pattern, is brought on by mutations in the APP, PSEN1, and PSEN2 genes, and APOE4 was discovered to be a significant risk allele for late-onset Alzheimer’s disease (LOAD) more than 20 years ago. Now, additional widespread variations at about 30 genetic loci have been discovered as a result of population-based genome-wide association studies of late-onset Alzheimer’s disease. Moreover, some genes have been found to contain uncommon variations that affect the risk for LOAD. These genetic developments have increased our understanding of the biological causes of Alzheimer’s. Additionally, presymptomatic people who are at risk for Alzheimer’s could be identified using the known genetic risk variations, which would further aid in the diagnostic evaluation of those who are actually symptomatic.

Treatment and Therapies
Genomics also plays a key role in precision medicine solutions for Alzheimer’s. Precision medicine aims to predict illness risk, understand disease origins, classify subtypes, enhance diagnosis, and personalize treatments using biological knowledge and health information. Integrating pharmacogenomics in clinical research enhances dementia diagnosis precision, allowing to tailors treatments, and accelerates medication development.
Already, findings from pharmacogenomics data have helped develop new therapeutics such as monoclonal antibodies, which are antibodies produced from a cell line made by cloning one unique white blood parent cell, as well as other small molecules that could potentially slow or stop the progression of Alzheimer’s. Ultimately, this is helping to extend the quality of life for those affected by the disorder and giving hope to their families. One example of this is the monoclonal antibody lecanemab, developed by Biogen, which binds to aggregated harmful amyloid beta proteins and helps clear them from the brain. It has been used in clinical trials, with some promising results—the treatment has been shown to improve cognitive performance in some patients with mild-to-moderate Alzheimer’s disease. A competitor, Genentech, also developed gantenerumab, a similar monoclonal antibody that did not perform as well.
While therapies are still in the early stages of development, the future is promising. With new technologies, including next-generation sequencing and supercomputing capabilities becoming increasingly available and affordable, the potential to identify novel treatments for Alzheimer’s is growing exponentially.
Researchers can accelerate discovery with g.nome®. Brought to market by a team of bioinformaticians, engineers and industry professionals, g.nome is a bioinformatic software that helps streamline genomic workflows. With a visual drag-and-drop pipeline builder that utilizes tools and pre-built workflows from a curated library, g.nome is giving power to researchers — enabling them to import custom code, handle big datasets reliably, and optimize team collaboration from anywhere.
With g.nome, long-time barriers linked to workflow language, process flow visibility, and quality control are removed. All that’s left are streamlined, scalable, and interoperable genomic workflows — leaving research teams to do what they do best: focus on the science.
Recent Developments in Genomics Research for Alzheimer’s:
- Researchers discovered hundreds of previously unknown and known Alzheimer’s disease-related genes using a deep learning framework called “network topology-based deep learning framework to identify disease-associated genes” (NETTAG), which combines multi-omic data sources and human protein interaction networks. Published in Cell Reports.
- According to a new study published in Nature Genetics, rare variations in the genes ATP8B4 and ABCA1 may raise the chance of acquiring Alzheimer’s disease. Researchers compared 16,036 people with Alzheimer’s disease against 16,522 controls who had all undergone exome sequencing for uncommon harmful mutations.
- Researchers compared gene expression and protein quantitative trait loci to reveal post-translational modifications that may be responsible for the onset and progression of Alzheimer’s. Using SomaLogic’s SomaScan technology, a professor of psychiatry at Washington University discovered 400 proteins and about 2,300 protein quantitative trait loci (pQTLs) associated with Alzheimer’s disease in samples of cerebrospinal fluid (CSF), brain tissue, and plasma. Published in Nature Neuroscience.
1. Nativio, R., Lan, Y., Donahue, G. et al.An integrated multi-omics approach identifies epigenetic alterations associated with Alzheimer’s disease. Nat Genet 52, 1024–1035 (2020). https://doi.org/10.1038/s41588-020-0696-0